Case #8: Automotive Acidosis
Author: Christopher Lim, MD
Peer Reviewer: Steve Aks, MD
A 36 year old male is brought by ambulance to the emergency department after his wife found him unarousable. His wife states that he has a history of alcohol abuse and was found with a bottle of automotive fluid next to him. During transport to the hospital, the patient has one seizure-like episode. He was intubated en-route and given midazolam.
Vitals: Temp: 98.6, HR: 112, RR: 28, BP: 106/70, O2 sat: 98% on 100% FiO2
ABG: pH 6.6, pCO2 33, PO2 253, HCO3 3.3
What is the most likely toxicologic etiology of this patient’s presentation?
The severe metabolic acidosis combined with suspected automotive fluid exposure suggests
toxic alcohol ingestion.
Toxic alcohols found in common household products include: methanol (classically associated with windshield wiper fluid), ethylene glycol (classically associated with antifreeze), diethylene glycol, propylene glycol, and isopropyl alcohol.
What other clinical symptoms or complications might you expect to see with this patient?
Mild ingestions produce inebriation similar to ethanol intoxication.
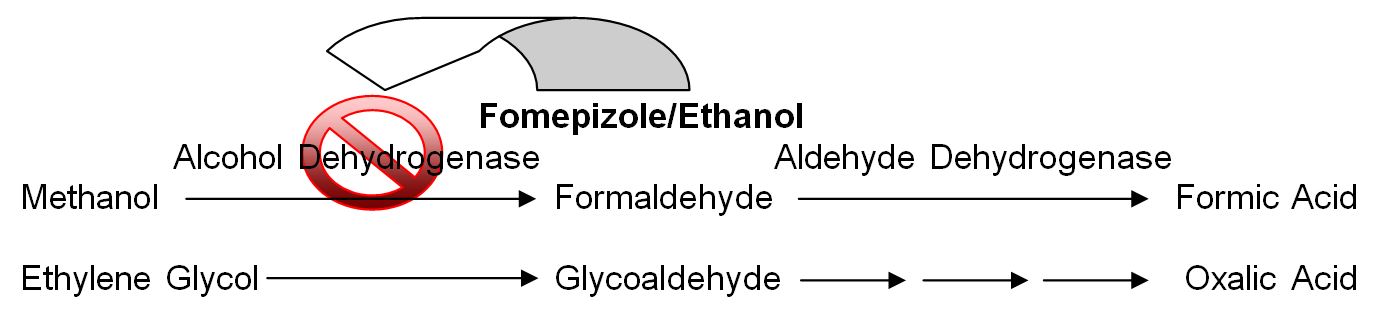
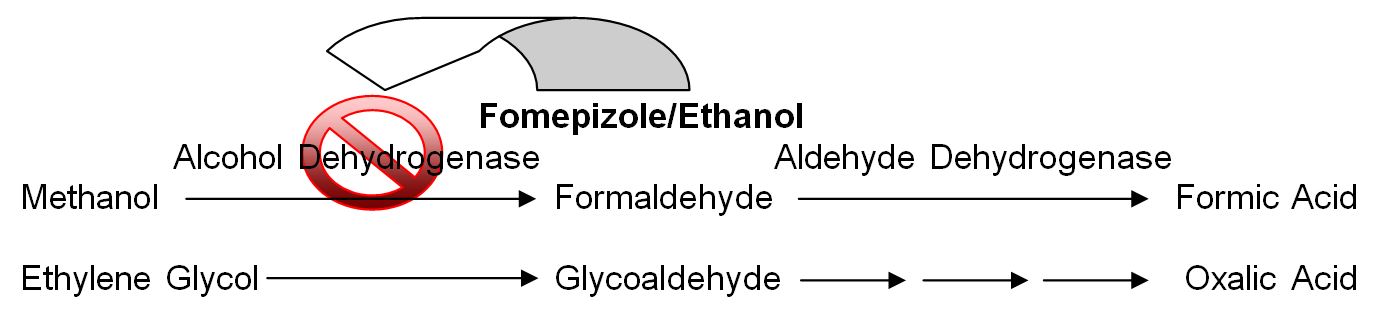
Severe anion-gap acidosis is the hallmark of toxic alcohol poisoning and results from toxic metabolites formed by the breakdown of ethylene glycol (oxalic acid) and methanol (formic acid).
Oxalic acid forms a complex with calcium and precipitates as calcium oxalate monohydrate crystals in the renal tubules, causing nephrotoxicity. Formic acid has a high affinity for the CNS, and in particular, the eye, resulting in visual disturbances.
What is the treatment for this patient?
Fomepizole or an alcohol drip (titrated to a serum ethanol level of 100 mg/dL) should be initiated as early as possible. Fomepizole and ethanol both work by inhibiting alcohol dehydrogenase, as shown below.
 However, the cornerstone of therapy is hemodialysis, which removes both the parent compound and toxic metabolite, and corrects any acid-base disturbance. Indications for hemodialysis include refractory acidosis, cardiopulmonary collapse, end-organ manifestations, or a concentration > 50mg/dL.
However, the cornerstone of therapy is hemodialysis, which removes both the parent compound and toxic metabolite, and corrects any acid-base disturbance. Indications for hemodialysis include refractory acidosis, cardiopulmonary collapse, end-organ manifestations, or a concentration > 50mg/dL.
Other adjunctive therapy includes sodium bicarbonate, thiamine (for ethylene glycol poisoning), pyridoxine (for ethylene glycol poisoning), and folic acid (for methanol poisoning).
What further work-up is required?
Testing includes BMP, ethanol/methanol/ethylene glycol levels, blood osmolality, urinalysis, ABG, and an ECG. Don’t forget to calculate the anion and osmolar gap (see below)!
Anion Gap Calculation: Na – (Cl + HCO3)
Osmolar Gap Calculation: Measured Osmolality – Calculated Osmolality
Calculated Osmolality: 2 x Na + (Glucose/18) + (BUN/2.8) + (Ethanol/4.6)
Measurement of methanol and ethylene glycol concentrations will confirm the diagnosis, but are often not immediately available. Measurement of ethanol concentration is important to note the presence of any ADH inhibition at outset. An ethanol concentration > 100 mg/dL makes toxic alcohol unlikely as the cause of an unknown anion gap metabolic acidosis. A high osmolar gap may suggest toxic alcohol ingestion, but has many limitations and is neither sensitive nor specific. A normal or negative osmolar gap does not exclude toxic alcohol poisoning. Patients with intentional ingestions should also have serum salicylate and acetaminophen concentrations determined.
What is the disposition of these patients?
The length of observation before discharge should be 6 hours in suspected ethylene glycol accidental ingestions and 12 hours in suspected methanol accidental ingestions. Any patient with mild symptoms or biochemical abnormalities should be admitted for further monitoring. Patients with severe signs and symptoms should be admitted to an intensive care setting. Patients without any sign or symptom of toxic alcohol ingestion during the period of observation can be discharged.
References:
Barceloux DG, Bond GR, Krenzelok EP, et al. American Academy of Clinical Toxicology practice guidelines on the treatment of methanol poisoning. J Toxicol Clin Toxicol. 2002;40(4):415-46.
Litovitz T. The alcohols: ethanol, methanol, isopropanol, ethylene glycol. Pediatr Clin North Am. 1986 Apr;33(2):311-23.
Return to Case List